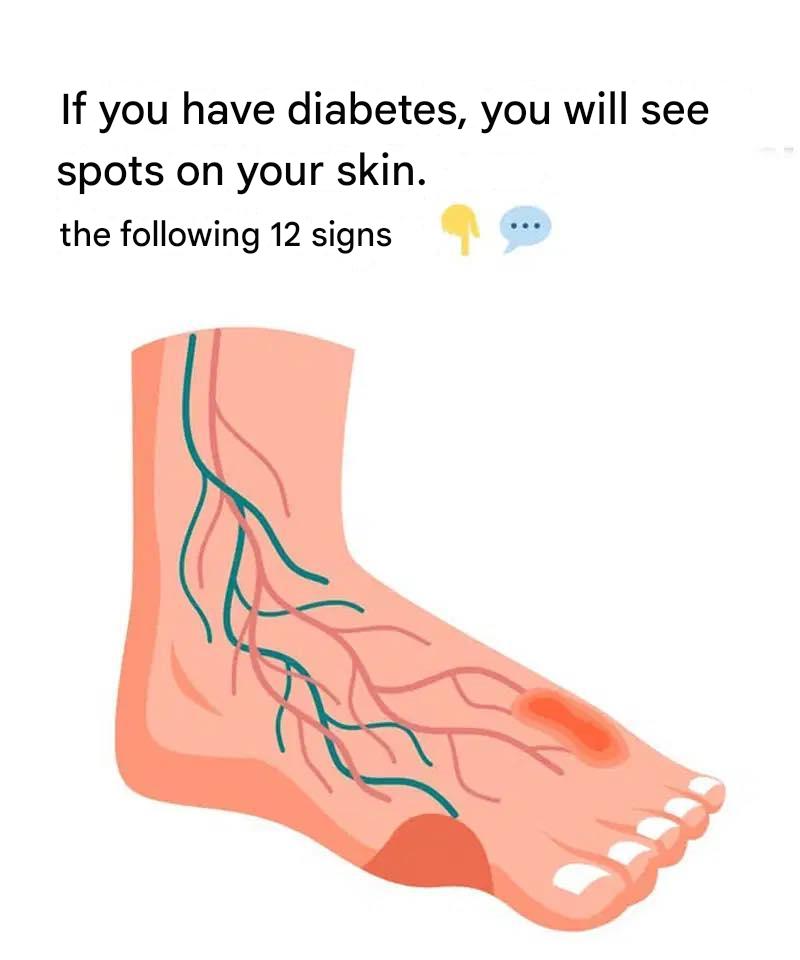
Have you ever noticed unexpected changes in your skin? For individuals living with diabetes—or those at risk—the skin can function as an early alert system. It often reveals subtle signals about blood sugar imbalance or insulin resistance long before other symptoms appear. Taking diabetes-related skin changes seriously is essential, as early recognition can lead to faster treatment and better outcomes.
In fact, nearly one out of three people with diabetes will develop a skin condition related to their disease at some point. That’s why it’s important to recognize these warning signs. Below, we explore 12 diabetes-related skin conditions that should never be ignored.
From persistent dark patches to sores that refuse to heal, this guide explains what these skin issues may indicate about your overall health. Understanding how diabetes can show up on your skin allows you to act sooner, seek proper medical care, and potentially prevent more serious complications down the road.
Common Skin Conditions Linked to Diabetes
Diabetes affects the body in many ways, and the skin is no exception. Often, it reflects internal health problems that might otherwise go unnoticed. Certain conditions—such as necrobiosis lipoidica, which causes shiny, raised patches, or acanthosis nigricans, known for dark, velvety skin in body folds—are closely linked to high blood sugar and insulin resistance.
Some individuals develop thickened or stiff fingers, while others experience diabetic blisters that resemble burn blisters despite no prior injury. Skin infections are also more frequent in people with diabetes, as weakened immunity and elevated glucose levels create an ideal environment for bacteria and fungi to thrive.
Fungal infections, such as athlete’s foot, often develop in warm, moist areas. Other conditions include diabetic dermopathy, which appears as light brown patches on the shins, and eruptive xanthomatosis, characterized by yellowish bumps surrounded by redness.